The Ask the Analyst series is a deep dive into the data by those most familiar with the CO APCD – the analysts themselves. We’ll hear about their experiences with recent analyses and answer any pressing questions that come up. Have a question for the CIVHC Analyst Team? Email it to info@civhc.org.
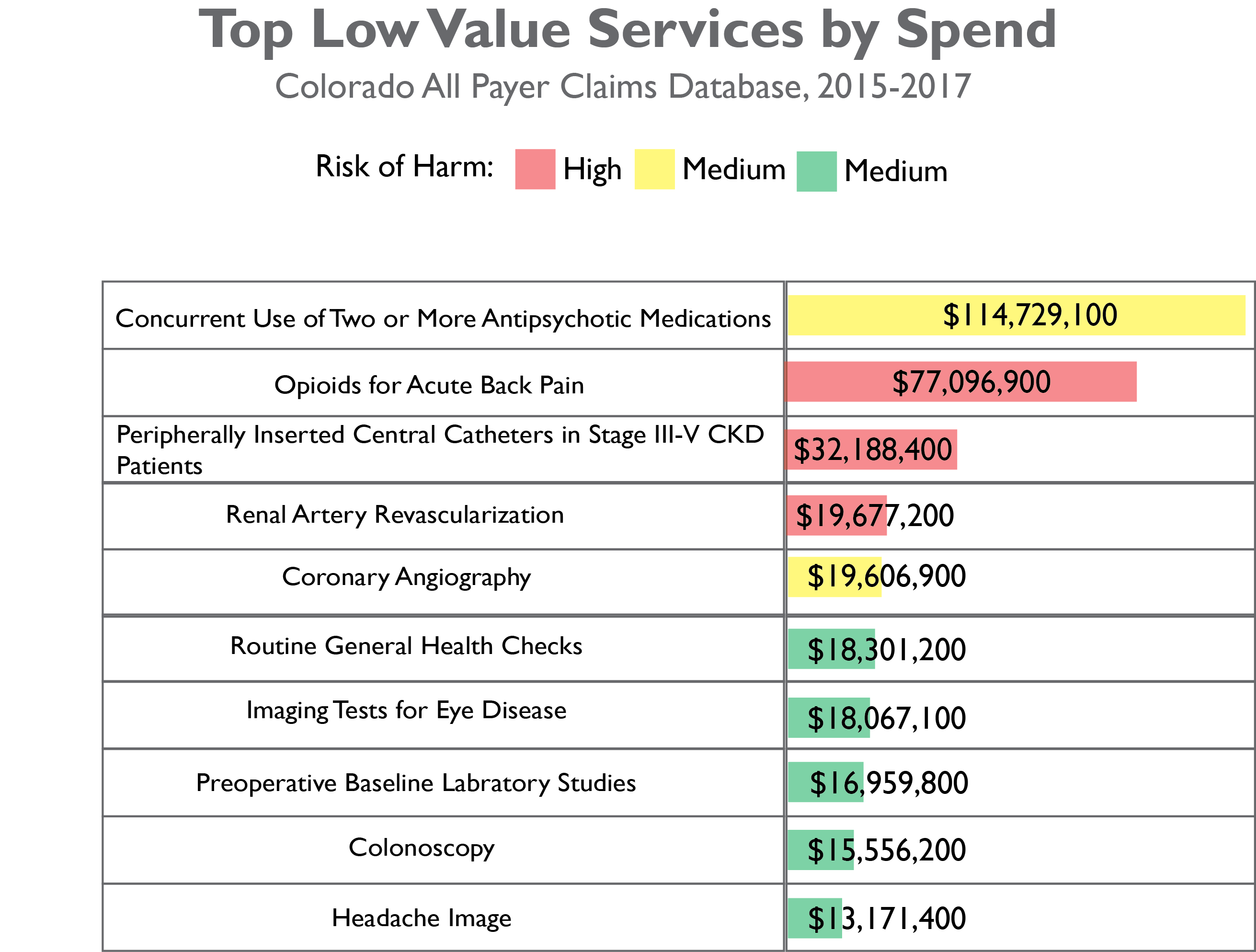
Featured Project: CIVHC’s report on low value care in Colorado processed health care claims from 2015-2017 for over 4.1 million people to determine the overall cost and volume of low value care in Colorado. Low value care is care in which the cost or potential harm to a patient is greater than the benefit.
Analyst Name: Tim Ginader, MS
- What were your first steps when beginning this analysis?
CIVHC worked with the actuarial firm Milliman to run the CO APCD claims from 2015-2017 through their MedInsight Health Waste Calculator, a low value care calculation tool. I took the data files we received from Milliman and processed them to prepare for analysis.
- Were there specific considerations you needed to consider based on the data?
I needed to consider how to take the raw data files from Milliman and analyze and report it in a meaningful way. We wanted to highlight the pervasiveness of low value care across the state, but also consider ways to reduce or eliminate it.
- What challenges did you encounter while performing the analysis? How did you overcome them?
There were many tough decisions that had to be made around how best to report the results. Do we include the cost of the entire claim in which low value care occurs, or just the claim line cost? Do we report the “top measures” by cost or volume? Ultimately, we decided the most accurate way to report the data was by claim line (to not artificially inflate costs) and to rank measures by spend (to prioritize measures with the greatest impact on quality of care and cost).
- Without delving into results, did anything surprise you about this analysis or the process of executing it?
I was very surprised by how widespread low value care is across the state. It affects all payers, all regions, and is performed by all types of providers.
- What did you learn while performing this analysis?
I learned a lot of medical care that is considered ‘routine’ is actually more harmful or costly to a patient than its anticipated benefits. There is a lot of opportunity to increase patients’ quality of care while lowering overall costs.