Unnecessary and Potentially Harmful Care Cost Payers and Patients $134 Million
Low value health care services are certain treatments, diagnostic tests, and screenings where the risk of harm or cost exceeds the likely benefit for patients. A new analysis released by the Center for Improving Value in Health Care (CIVHC) shows that in 2020, Coloradans received over one million unnecessary and potentially harmful low value health care services resulting in $134 million in excess cost for Coloradans and health insurance companies. Compared to 2019, the number of low value care services and total spending decreased, yet the percent spending that was identified as low value care, of the services evaluated, increased by almost 9%.
The low value care analysis is part of the recently released Affordability Dashboard and is the second analysis to be added to the tool in addition to cost of care information. Low value care services were identified by applying 2017-2020 claims in the Colorado All Payer Claims Database (CO APCD) to the Milliman MedInsight Health Waste calculator software. Medical boards, specialty societies and providers have collectively identified low value services, available in the Choosing Wisely guidelines. This analysis includes 48 potentially low value services that can be evaluated using claims data.
Across all payers, the top 10 services by spend accounted for 77% of the state’s total low value care spending and included: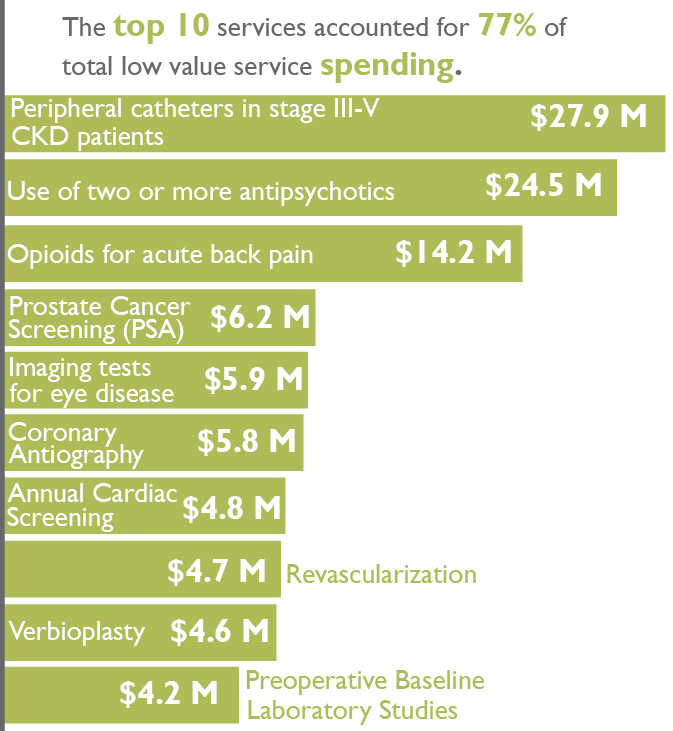
- Peripheral catheters in late state kidney disease patients ($28M)
- Use of two or more antipsychotic medications ($25M)
- Opioids for acute back pain without trial of alternative medications ($14M)
- Routine prostate cancer screening in men with no symptoms of disease ($6M)
Results show that the average cost for a low value care service is $130. However, the top service by spend, peripheral catheters in late stage kidney disease patients, costs over $14,000 per incidence and has a high risk of actually harming patients. The use of two or more antipsychotic medications, the second highest total spend low value care service, costs patients and their insurance companies nearly $400 for each event.
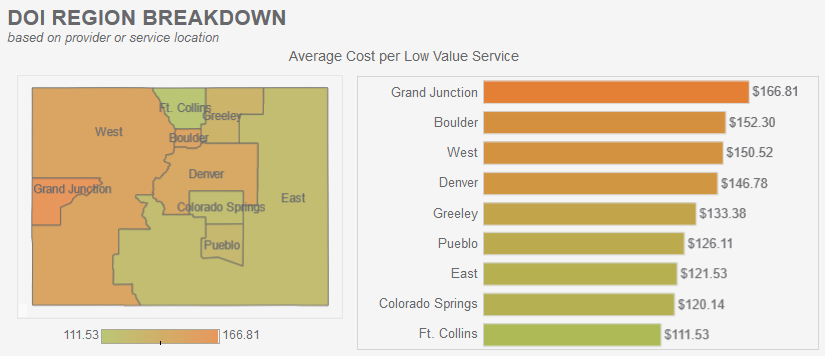
The interactive capabilities of the report allow users to filter by health insurance payer type, and drill down into cost by Division of Insurance (DOI) region across the state. The Grand Junction region has the highest average cost per low value service ($167), with over $2M in spending in 2020 going towards prescribing patients with two or more antipsychotic medications.
“Reducing potentially unnecessary care is something patients and providers can readily address together, and doing so would have profound benefits on both cost savings and overall health of Coloradans,” states Ana English, President and CEO of CIVHC. “The low value care data helps identify specific services and areas we should consider addressing together as a state.”
Efforts to reduce low value care that have proven effective in other states include provider-focused and patient education interventions as well as multi-stakeholder collaborations. Successful initiatives tailor strategies to address each unique low value care service as each needs to be evaluated based on the patient diagnosis and history, patient expectations regarding treatment, and payment incentives.
This analysis provides valuable information for many stakeholders looking for areas of improvement in cost savings and quality of care, and makes the case that opportunities exist. CIVHC is able to provide data specific to providers, payers, employer groups, and others necessary to inform improvement activities at the local community level. If you are interested in understanding low value care for your employee, member, or patient population, please contact us at info@civhc.org.
Related Resources: