Impact of Respite Care for Persons Affected by Alzheimer’s Disease and Related Dementia
Many are familiar with Alzheimer’s disease, a brain disease that deteriorates your memory and other mental functions. According to the Alzheimer’s Association, every 65 seconds someone in the US develops Alzheimer’s, and it is becoming more prevalent throughout the country. In spite of many years of research, Alzheimer’s has no known cure, which often leaves friends and family responsible to care for those impacted for many years.
As time progresses, so does the severity of the disease, which increases the workload and stress for caregivers who provide informal care and support. People affected by Alzheimer’s often need round the clock attention and support, and as a result, caregivers have higher rates of stress, depression, anxiety, physical ailments, increased cardiovascular disease and weakened immune systems.
Respite care is a way to provide care for those living with Alzheimer’s and dementia, giving caregivers some temporary relief. Respite care comes in a variety of services and durations including in-home, adult day care, and short nursing facility stays. However, many families and caregivers are unaware that these services exist.
In an effort to expand the use of respite care by caregivers, Dr. Sean Reed and Dr. Hillary Lum, researchers at the University of Colorado Anschutz Medical Campus in the College of Nursing and School of Medicine Division of Geriatric Medicine, began investigating the impact of respite care on caregivers and patients. In addition to health and well-being, because Alzheimer’s and dementia are very costly diseases with over $300 billion being spent on care in 2020, the researchers also wanted to understand how respite care impacted use of high cost services such as hospitalizations and Emergency Department visits.
With these goals in mind, CU researchers accessed a Custom Data Set from the Colorado All Payer Claims Database (CO APCD) to answer the following questions:
- Among older adults with and without dementia, what is the prevalence of respite care use?
- What is the association of use of respite care for beneficiaries with or without a diagnosis of dementia on long-term care nursing home admission or mortality?
- What are the patterns of respite care use among individuals with dementia, including other long-term services and supports and health care utilization (ED visits, hospitalizations, clinic visits, post-acute care)?
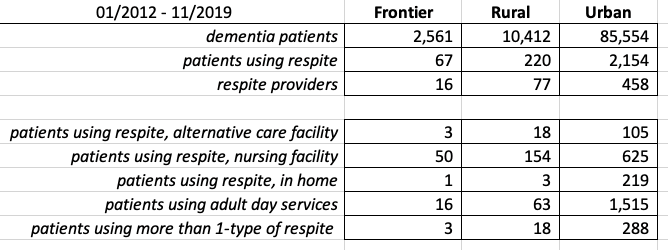
From the CO APCD data set, of the 98,527 patients with a diagnosis of dementia, less than 3% used respite services during 01/2012 – 11/2019. Ongoing work includes utilizing the Colorado Rural Health Center’s County Designations classification to help investigate potential disparities in respite services between frontier, rural, and urban counties. Initial findings suggest only 287 out of 12,973 patients took advantage of respite care in their frontier and rural communities, while 2,154 out of 85,554 patients used respite in urban counties. Overall, patients utilizing respite care fell into the following categories:
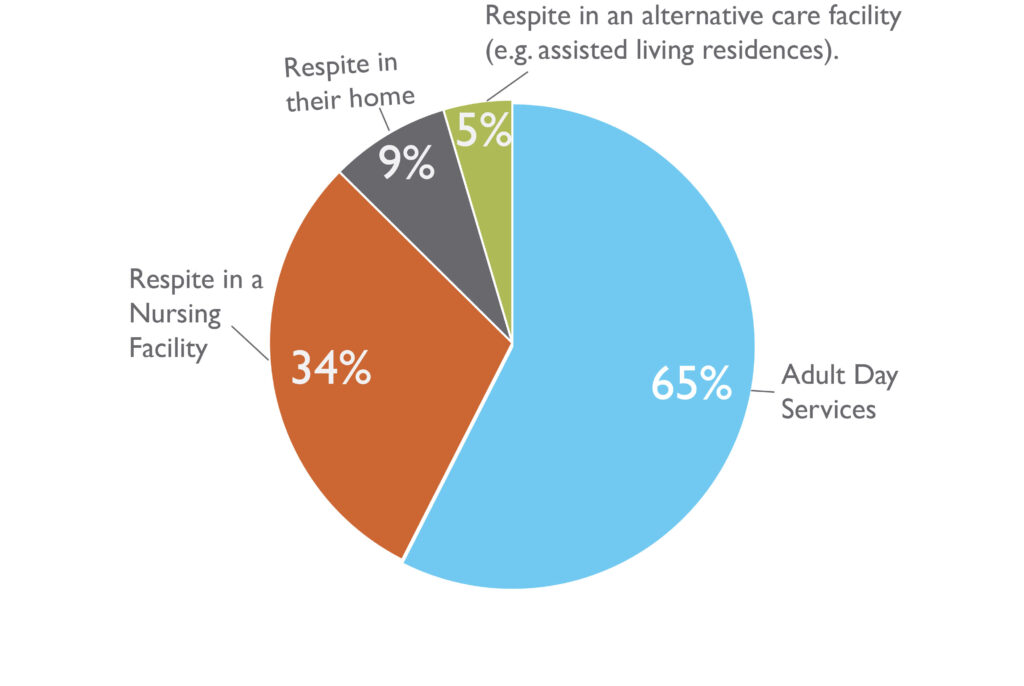
Only 12.7% of respite patients utilized more than one type of respite service.
While no cure for Alzheimer’s exists, there are ways for patients and families to receive support to help cope with this devastating disease, that not only impacts the person living with the disease, but their entire support network as well. Respite care services have yet to be fully utilized by those needing it most, but have the potential to lower long term medical costs, provide relief to essential primary caregivers, and ensure care and safety to those affected by Alzheimer’s or dementia. Findings from this project, which is currently underway, have the potential to help better understand the preferences, availability, access and other factors that may influence the future use of respite care.
For more information, contact Dr. Sean Reed: sean.reed@cuanschutz.edu