Health care costs are rising rapidly across the country, and Colorado is not exempt – a previous analysis using data from the Colorado All Payer Claims Database (CO APCD) found that cost of care in our state increased by 13% from 2013 to 2019.
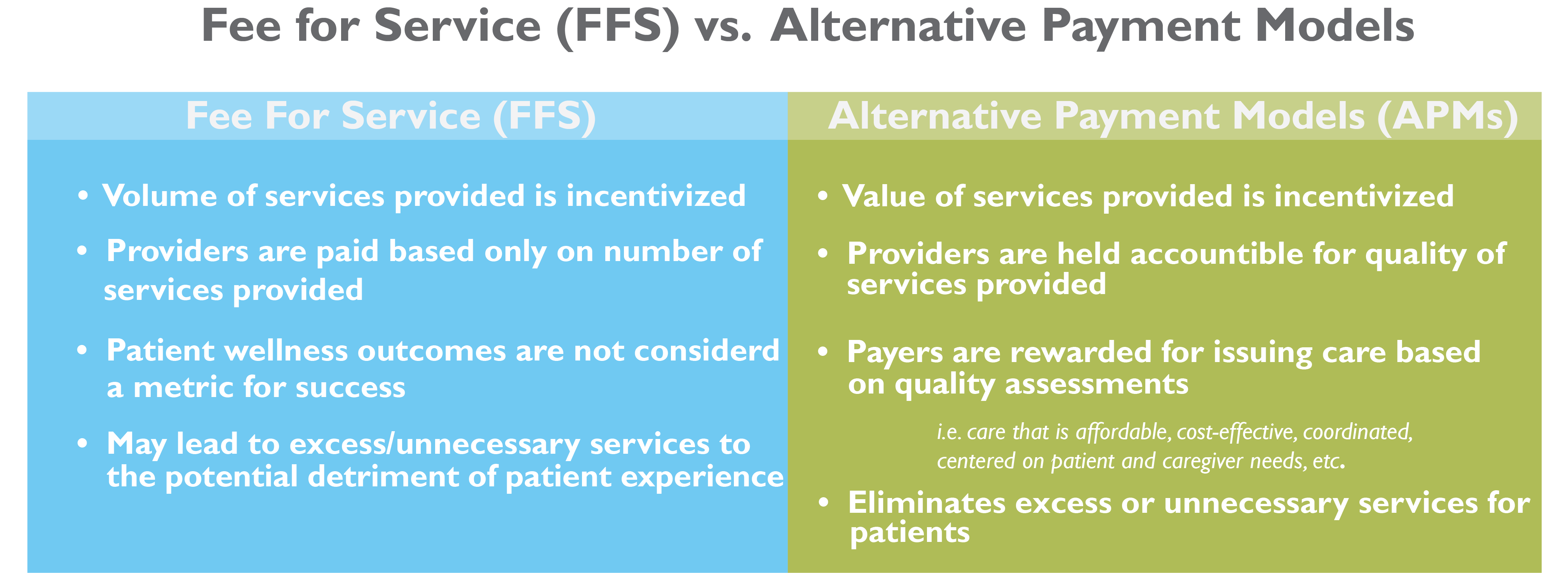
To address rising costs, there are efforts underway to change the way health care is paid to incentive providers and health systems to lower costs and improve quality of care. Shifting away from the current Fee-for-Service system towards Alternative Payment Models (APMs) reimburses providers in a way that supports delivering more efficient, cost-effective, high-quality care.
Colorado is taking steps towards transitioning to APMs through various initiatives and legislative efforts. To track progress towards integration, the CO APCD became one of the first in the country to begin collecting data on APMs in 2019. Recently, CIVHC released the first analysis on APMs in Colorado on the Affordability Dashboard, showing where our state stands on building a better payment system.
Why APMs Over Fee-For-Service?
Since the 1930s, the health care system has operated under a fee-for-service (FFS) model, which pays providers based on the number of services provided. This encourages doctors and hospitals to see more patients more often so they can bill for more services which ultimately increases health care costs. APMs, however, generally offer providers a fixed amount of money with which they can use at their discretion to provide services and keep patients healthy.
To better understand APMs vs. FFS, it’s helpful to have an example. Let’s imagine that Doctor A gets paid through an APM model, and is given $200 per month to take care of you regardless of how many times she sees you or how. Doctor B, on the other hand, is still on a FFS payment model and only gets paid when you actually have a visit with her. One day, you wake up with what you suspect is pink eye. If Doctor A is your provider, you could call her office or email her through a patient portal, and based on your symptoms, she could confirm you have pink eye and send a prescription for eye drops to your pharmacy. Doctor B, however, doesn’t get paid unless you come into her office or have a telehealth visit, so you have to make an appointment and physically or virtually get seen before she can get reimbursed. In this scenario, Doctor A didn’t have to open up a spot on her busy schedule that day to see you, and you didn’t have to take time off work for a doctor’s visit. This efficient more cost-effective model of care is a win for both you and your provider.
So why don’t all doctors and hospitals get paid this way? It’s not as easy as it seems to change from FFS to an APM model. Payers have complex electronic billing and payment systems set up don’t easily convert to an APM model, and providers also have current processes and delivery systems set up that take time and resources to change. And, there is a reason we’ve been saying “APMs” with an “s”! There are multiple types, and some work better for some providers, patients and services than others.
Types of APMs
Since not all APM models are the same, and implementing new payment models is difficult to do and track, the Health Care Learning and Action Network (HCP LAN) was developed to help measure and support adoption of APMs. According to HCP LAN, adoption of APMs is increasing with 41% of health care payments flowing through APMs according to their 2021 report.
To guide the complicated process, the HCP LAN breaks APMs into four stages of implementation, each seen as stepping stones to the ultimate goal of stage four, which provides payments for an entire population (aka all the patients a doctor sees), all tied to quality and health outcomes.
Payers who submit APM data to CIVHC are required to submit their APM data in one of the categories which allows us to report data that aligns with HCP LAN national reporting.
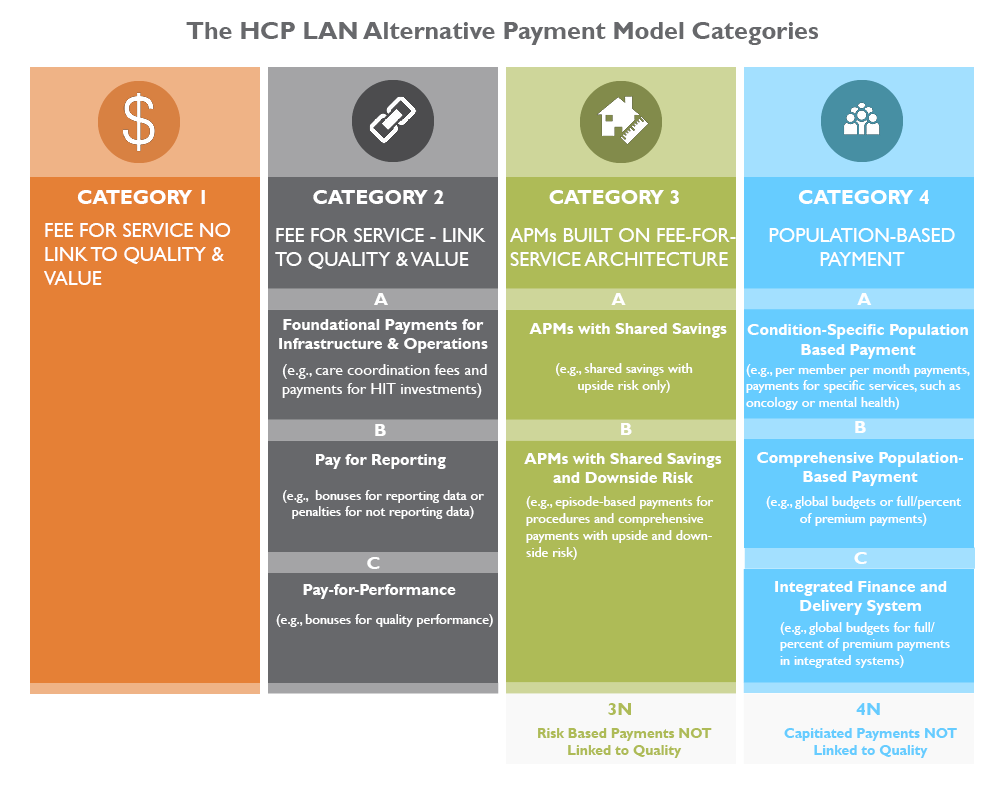
To view detailed guidelines behind this framework, review HCP LAN’s refreshed 2017 APM Framework white paper.
APMs In Colorado
Overall, in Colorado, the percent of health care payments that are getting paid through an APM is decreasing according to the latest data from 2018-2020, while the percent of APM payments specifically for primary care providers remains stable. The majority of payments across all payers are in the 2C category (pay for performance), while among commercial payers most are in the 3A category (shared savings). Through CIVHC’s interactive dashboard you can look at the APM information in a number of ways, and our infographic and issue brief are also available to help you understand the data.
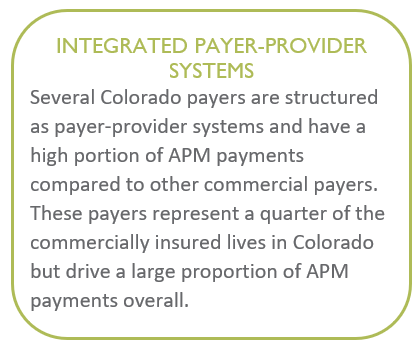
When viewing CIVHC’s APM dashboard, it is important to understand that you can look at the data both with and without integrated payer-provider systems and non-value based payments. Integrated payer-provider systems are health systems like Kaiser, for example, who are both a provider of health care and a payer simultaneously. These systems are already designed to pay through an APM model, and therefore increase the APM percentages when they are included.
Non-value based payments (categories 3N and 4N) represent APM payments that have no link to quality, so you can determine if you want to look at only APMs that consider patient outcomes or exclude them when viewing the report.
The Value of APM Data
Colorado is well-positioned to continue as a leader in APM adoption given statewide programs and initiatives. Current state efforts to encourage payment reform have identified APMs as a crucial mechanism of larger systemic change with significant backing at the legislative level.
The CO APCD APM data is supporting new legislative policies aimed at improving care and lowering costs. In 2019, HB19-233 was established to increase investments in primary care in Colorado to ultimately improve access and lower costs. The bill established the Colorado Primary Care Reform Collaborative charged with making annual recommendations to increase access to coordinated primary care. To support the development of the Collaborative’s recommendations, CIVHC submits an annual progress report on primary care and APM spending to help them understand current health care spending for primary care overall and through APMs.
In 2022, the Colorado General Assembly passed HB22-1325 requiring the DOI and HCPF to develop rules for APMs for primary care in the commercial market. The bill requires CIVHC to work with the DOI to develop and report on quality measures starting in 2024. CIVHC will continue to partner with the Collaborative, DOI, and other organizations to provide insight on APM spending to help determine a pathway to make investments that will improve outcomes and lower costs for Coloradans.
Learn more: