PROFILE: The Chambers Hope Health and Wellness Clinic
![]() Click here to listen to CIVHC’s Chief Medical Officer, Jay Want, MD chat with Lauren Tolle, Ph.D., Division Director for Integrated Care at Aurora Mental Health Center and Margie Kaems, LCSW, Clinical Social Worker and Program Manager of the Hope and Health Wellness Clinic and the Mobile Heart Health Project.
Click here to listen to CIVHC’s Chief Medical Officer, Jay Want, MD chat with Lauren Tolle, Ph.D., Division Director for Integrated Care at Aurora Mental Health Center and Margie Kaems, LCSW, Clinical Social Worker and Program Manager of the Hope and Health Wellness Clinic and the Mobile Heart Health Project.

Founded in 1975 by residents determined to bring services to their city, the Aurora Mental Health Center (AUMHC) began in a donated space. In the 42 years since inception, the center has grown to over 400 employees, 16 specialty clinics, seven counseling centers, six residential facilities, and an active presence in public schools and homes across Aurora. Guided by their commitment to create healthy and secure communities by providing the least restrictive service that ensures quality, appropriate, and efficient care, the center believes that everyone should have the opportunity to live full and rewarding lives, unhampered by mental illness.
 Project Summary: AUMHC opened the bidirectional, Chambers Hope Health and Wellness Clinic in 2013, in partnership with their Federally Qualified Health Center partner, Metro Community Provider Network. The clinic is designed to serve adults, many of whom are clients of AUMHC, struggling with serious and persistent mental illness, through integrated primary, behavioral health care, and comprehensive wellness services.
Project Summary: AUMHC opened the bidirectional, Chambers Hope Health and Wellness Clinic in 2013, in partnership with their Federally Qualified Health Center partner, Metro Community Provider Network. The clinic is designed to serve adults, many of whom are clients of AUMHC, struggling with serious and persistent mental illness, through integrated primary, behavioral health care, and comprehensive wellness services.
The clinic’s multidisciplinary team supports individuals’ health and wellness through a number of different resources, including:
- Individual behavioral health interventions,
- Care coordination, connecting patients with outside specialty care referrals as well as support in accessing community resources including transportation, benefit assistance, housing and food resources,
- A weight loss group, using an empirically-supported curriculum for individuals with serious mental illness
- Access to a fully-equipped, onsite fitness center and personal trainer who works with individuals on their fitness plans,
- A chronic pain group,
- An Cognitive Behavioral Insomnia group, and
- Healthy cooking classes through partnership with Cooking Matters.
Additionally, through support from the Substance Abuse Mental Health Services Administration (SAMHSA)’s Primary and Behavioral Health Care Integration (PBHCI) initiative, the clinic is able to offer an incentive program for individuals working toward their health goals who need additional support. This support includes passes to the local recreation center, gift cards to help with purchasing appropriate clothes and shoes for exercising, nicotine replacement therapies, cookbooks for suggestions on eating healthy on a budget, and health tracking equipment like pedometers and jump ropes to assist people in monitoring their healthy activities.
Successes: Building a new system to refer mental health clients to a bi-directional integrated primary care clinic took time and perseverance. Clinic staff began by forming relationships with mental health care providers, conducting trainings and participating in team meetings to help mental health clinicians remember to assess their clients’ access to and need for primary care services. They also had to work to engage patients in the clinic, many of whom had not seen a primary care provider in decades. It was necessary to get patients to trust the medical providers and the integrated care team. Once trust was established, the clinic staff guided the patients to start thinking about changing unhealthy behaviors, like smoking, or to begin making healthy lifestyle choices, like exercising. Since opening in January, 2013, over 1,500 adults with serious mental illness have been referred to the clinic.
Challenges: The biggest challenge faced by the clinic team has been finding the balance between focusing on improving patients’ health and wellness while ensuring that these individuals also have the resources to meet their most basic needs. Some of the clinic’s patients face chronic homelessness, food insecurity, or financial hardships; and while the clinic’s care coordinator is available to assist with many of these challenges, there are not always easy solutions. In addition, many individuals served in the clinic have gone without medical care, or have had inconsistent or fragmented care, increasing risk of undiagnosed or poorly managed chronic conditions.
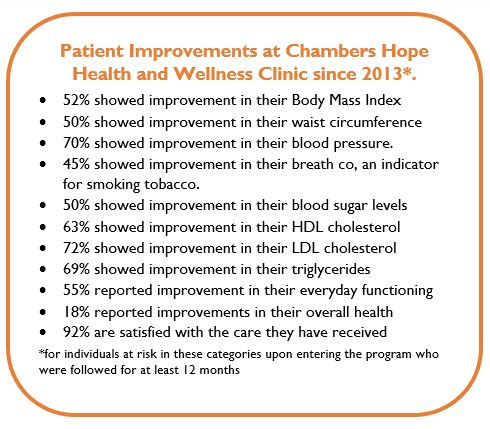
Impact: Many patients have successfully quit smoking, lost substantial amounts of weight, and experienced overall improvements in their health. One example is a 59 year old female client who presented to the clinic wanting to lose weight but struggled with emotional eating and was anxious to leave her home. After working with the behavioral health providers to build awareness of her eating habits and build confidence around physical activity, she has successfully lost 60 pounds and is walking at least 10,000 steps a day outside. She attributes her success in part to the supportive, nonjudgmental and whole-person care she received from the team.
Aurora Mental Health Center wishes to acknowledge their wonderful community partners including: Metro Community Providers Network, Aurora Research Institute, Boomers Leading Change in Health, Dental Life Line Network, Colorado’s Project ECHO for chronic pain program, University of Colorado School of Nursing, University of Colorado’s Clinical Health Psychology program, University of Denver’s Social Work program, Kaiser Permanente’s Weigh and Win program, and Share Our Strengths’ Cooking Matters.