Overview
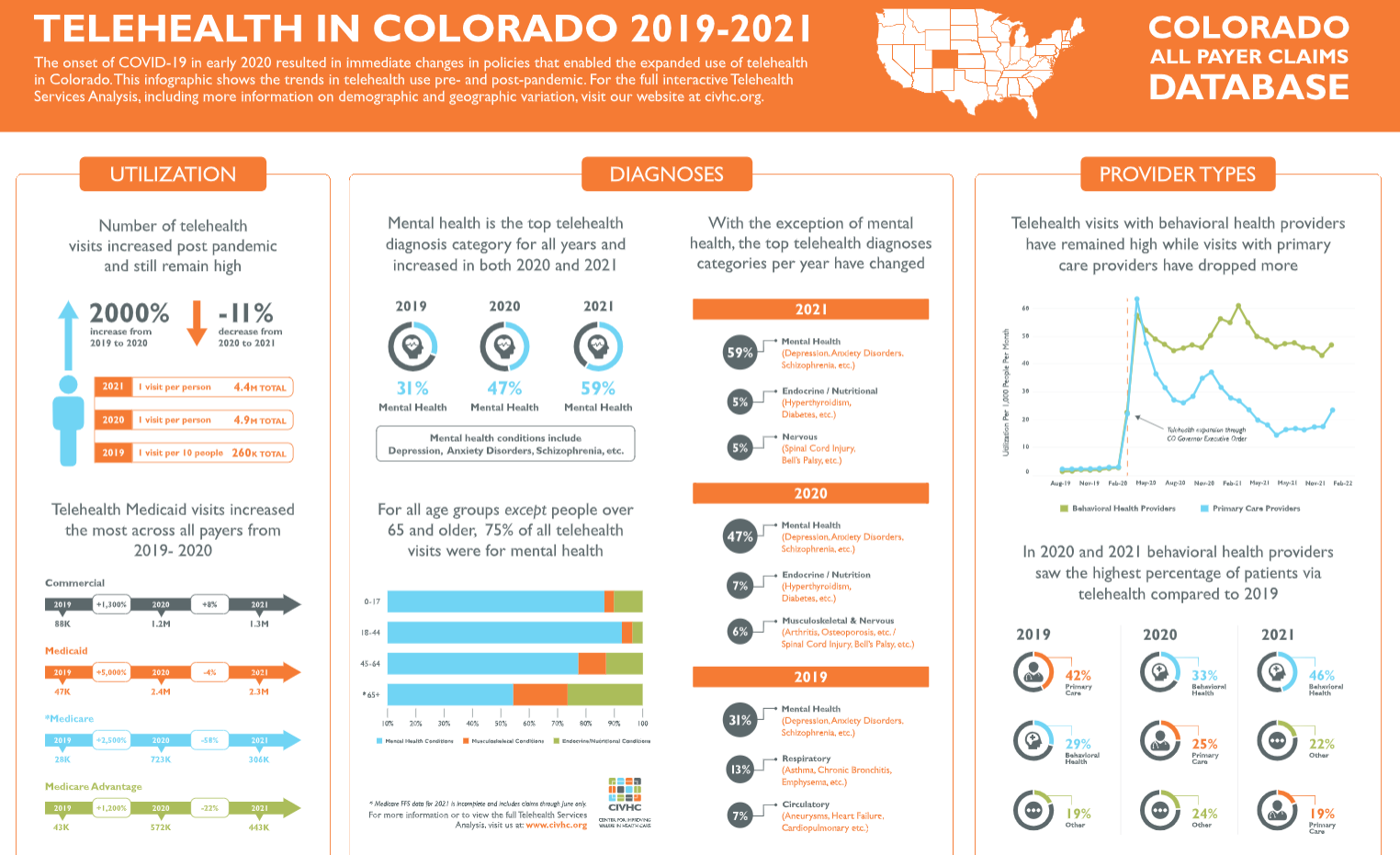
The Telehealth Services Analysis provides stakeholders with information to understand telehealth services prior to the onset of COVID-19, and the impact the pandemic has had on telehealth service use since March 2020. This report is updated regularly to enable users to track trends in telehealth services over time and the impact on cost and utilization. Please contact us at info@civhc.org for questions.
Learn More
Key Considerations
- Medicare Fee-for-Service is only available through June 2021; please use caution when viewing Medicare FFS or selecting “All Payers” for 2021.
- This analysis includes the majority of insured lives in Colorado, but does not include all self-insured employer covered lives, or federal health insurance programs such as the Veterans Administration, Tricare, and Indian Health Services.
- When viewing the data by provider type, Federally Qualified Health Center and Rural Health Clinic information is lower than expected because the analysis only captures visits when they are billed under their facility taxonomy and does not capture providers billing under a different taxonomy code (i.e. primary care).
- This analysis includes visits paid for through fee-for-service only, and do not include any supplemental payments or visits/payments that occurred through Alternative Payment Models.
Quick Links
Report Resources
- Overview and Methodology
- Report Update Press Release (released: November 30, 2022)