CO APCD Overview
The Colorado All Payer Claims Database (CO APCD) was recommended by the Governor-appointed Blue Ribbon Commission on Health Reform (208 Commission) and was created by legislation passed in 2010. CIVHC was named administrator of the CO APCD by the Executive Director of the CO Department of Health Care Policy and Financing (HCPF) the same year and the database was launched in 2012.
- CIVHC & CO APCD Timeline (through 2017)
- CO APCD Annual Reports
- Legislative Resources
How the CO APCD Works
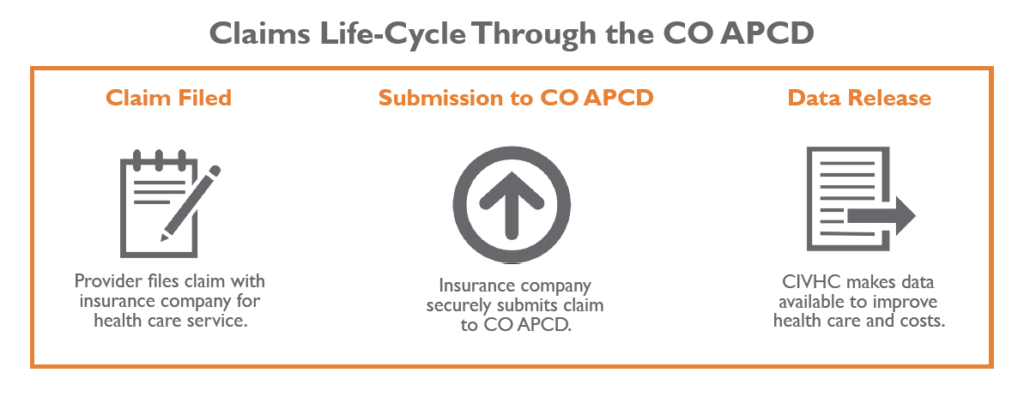
- A health care provider submits a claim for payment to the health insurance company or other payer (Medicare, Medicaid).
- This claim contains important information including charges, diagnosis, location, and services rendered.
- After processing the payment, the insurance company securely submits the claims information to the CO APCD.
- CIVHC processes these claims and turns them into public and custom information about how Colorado is paying for and receiving health care.
What’s in the CO APCD
The CO APCD is the state’s most comprehensive source of health care insurance claims information representing the majority of covered lives in the state across commercial health insurance plans, Medicare (Fee-for-Service and Advantage), and Health First Colorado (Colorado’s Medicaid program).
For searchable information on number of people, claim types and payers represented in the CO APCD, visit our CO APCD Insights Dashboard.